- Figure 1
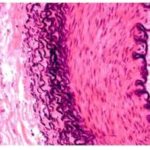
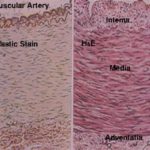
- Figure 2
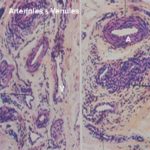
- Figure 3
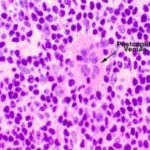
- Figure 4
- Figure 5
- Figure 6
- Figure 7
- Figure 8
- Figure 9
- Figure 10
- Figure 11
- Figure 12
- Figure 13
- Figure 14
- Figure 15
- Figure 16
Cardiovascular system
The cardiovascular system is made up of the heart and the various types of blood vessels and lymph vessels.
The principal functions of the cardiovascular system are:
Transport of oxygen and nutrients to the tissues.
Removal of carbon dioxide and other metabolic waste product from the tissues.
Plays a role in body temperature regulation.
Distribution of hormones and immune cells throughout the body.
Basic structure of the cardiovascular system
The wall of any blood or lymph vessels is made up of three layers or tunicae:
- Tunica intima
It is the innermost layer and consists of endothelium, subendothelium and internal elastic lamina.
The endothelium is a single layer of extremely flattened epithelial cell rest on a basement membrane.
The subendothelial layer is a delicate connective tissue layer contains collagen fibers and sheets of elastin.
The internal elastic lamina is a thin layer of elastic tissue separating the intima from the media and is especially prominent in muscular arteries.
- Tunica media
It constitutes the middle layer and consists of concentric layers of smooth muscle and elastic connective tissue. It is thick in arteries, thin in veins. It is formed of smooth muscles in muscular arteries and elastic membranes in elastic arteries.
- Tunica externa or adventitia
It is the outermost layer and consists of connective tissue layer of fine elastic and collagen fibers. It is separated from the media by external elastic lamina. The tissues of the wall receive their nutritional support by small arteries called vasa vasorum (e.g. vessels of vessels). These vessels are especially prominent in large veins and elastic arteries.
Arterial system
The primary function of the arterial system is to distribute blood from the heart to capillary beds throughout the body. The arteries are classified according to their size and structure into: large or elastic artery, medium-sized or muscular artery and arteriole or small artery.
The elastic arteries include the aorta, common carotid, subclavian arteries. The wall of the elastic artery is made up of tunica intima, tunica media and adventitia.
The tunica intima consists of endothelium, subendothelium and internal elastic lamina. The endothelium is a single layer of flattened endothelial cells rests on a thin basal lamina. The subendothelium is a thin layer of collagenous connective tissue containing few elastic fibers, scattered fibroblasts and smooth muscle-like cells known as myointimal cells. With increasing age, lipid may accumulate in the cytoplasm of the myointimal cells leading to atherosclerosis. The internal elastic lamina is indistinct.
The tunica media is the thickest of the three tunics and consists primarily of concentrically arranged, fenestrated elastic laminae separated by collagenous connective tissue and relatively few smooth muscle fibers. The external elastic lamina is indistinct. The tunica externa is a collagenous connective tissue layer with few elastic fibers and fibroblasts. Vasa vasorum and nervi vasorum are prominent.
They are also called distributing arteries because they are the main distributing branches to the various body regions.
The tunica intima consists of endothelium resting on a basal lamina. The subendothelium is a thin connective tissue layer with few fibroblasts and few smooth muscle cells. The internal elastic lamina is thick and fenestrated.
The tunica media: is the thickest layer composed of 2-40 circular layers of smooth muscle cells. A few elastic fibers and collagen fibers are scattered in between the smooth muscle. The media is separated from the adventitia by discontinuous external elastic lamina.
The tunica adventitia consists of elastic and collagenic fibers with vasa vasorum and nervi vasorum.
They are arterial vessels with a luminal diameter less than 0.3 mm. The tunica intima is very thin and comprises endothelium, subendothelial layer of a thin collagen and elastic fibers that are absent in small arterioles and Internal elastic lamina, which is thin but distinct.
The tunica media is composed of six or less circular smooth muscle layers. The external elastic lamina is absent.
The tunica adventitia is a connective tissue layer has the same thickness as the tunica media and merges with the surrounding connective tissue.
- Metarterioles and precapillary sphincter
Metarterioles
They are the smallest arterioles with a diameter of less than 40 μm. The tunica media is formed of isolated bundles of smooth muscle cells. They are divided into two segments; a proximal segment from which many capillaries may arise, and a distal segment known as thoroughfare channels that connect directly with venules.
Precapillary sphincter
It is formed of few smooth muscle cells that encircle each capillary at the site of its origin from arterioles.
Contraction of the smooth muscle within the wall of the arterioles, metarterioles and precapillary sphincter regulates the blood flow through the capillaries.
- Capillaries
They are thin-walled vessels with a diameter of 4-10 mm. The capillary wall is composed of endothelial cells, a basal lamina and pericytes.
The pericytes are relatively undifferentiated cells of mesenchymal origin that may differentiate into fibroblasts or smooth muscle when the needs arise. A network of capillaries known as capillary beds usually extends throughout all tissues and organs.
The capillaries are primarily concerned with exchange of gases (O2 and CO2), Fluids, nutrients and metabolic waste products between blood and tissues.
Types of capillaries
They are the most common types of capillaries in the body tissue (muscular and neural capillaries).
The capillary circumference is formed of one or more endothelial cells whose edges are sealed together by tight junctions or fascia occludens. The endothelial lining is continuous without any interruptions or fenstrations. Exchange between the lumen and the surrounding tissues occur by:
Passive diffusion. For example gases and small ions.
Pinocytotic vesicles. Example proteins and some lipids.
Passage between the intercellular space. Example white blood cells.
They occur in small intestine, endocrine glands and kidneys. The endothelial cells are perforated by fenestrations or pores traversed by diaphragms. The basement membrane is continuous across the fenestrations. Their permeability is much greater than that of continuous capillaries. The pericytes are rarely found around their endothelium.
- Discontinuous capillary
They occur in liver, bone marrow and spleen. The basal lamina is discontinuous across the pores or fenestrations leaving a wide gap within the endothelial lining.
The blood sinusoids are capillaries of wide diameter and irregular outline. They are more permeable than capillaries and are found in the liver, spleen, bone marrow and some endocrine glands.
The endothelium of the sinusoids may be continuous, fenestrated or discontinuous.
The basal lamina is discontinuous or absent. Macrophages are usually associated with their walls.
The venous system
The primary function of the venous system is to return blood from the capillaries to the heart.
Veins are classified according to their size and structure into:
They are endothelial tubes slightly wider than capillaries (about
30 μm in diameter). Pericytes and little connective tissue surround them.
Functions
Exchange like capillaries.
They are the main sites at which white blood cells leave or enter the circulation.
- Collecting venules
The post-capillary venules drain into collecting venules. They are slightly larger with a greater number of pericytes.
- Muscular venules (small veins)
The tunica intima consists of endothelium rests on basal lamina. The internal elastic lamina is absent.
The tunica media consists of one or two layers of smooth muscles.
The tunica adventitia is a thin connective tissue layer continuous with the surrounding connective tissue.
The muscular venules are similar to arterioles except;
They have a wide diameter relative to the thickness of the wall.
The lumen is usually collapsed and filled with blood.
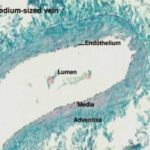
The tunica intima consists of endothelium rests on basal lamina. The subendothelial layer is thin and consists of collagen and elastic fibers.
The internal elastic lamina is absent.
The tunica media is thinner than adventitia and consists of few layers of smooth muscle cells.
The tunica adventitia is much thicker than media composed of collagenous fibers with few elastic fibers.
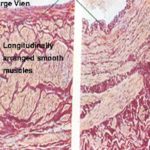
The tunica intima consists of endothelium and a prominent subendothelial layer. The tunica media: is thin compared to the diameter of the lumen and consists of a few layers of smooth muscle cells separated by bundles of collagen fibers.
mooth muscle may be entirely absent.
The tunica adventitia is the thickest layer and composed of longitudinally arranged bundles of smooth muscle cells with collagen and elastic fibers.
The veins of the extremities that are working against gravity are equipped with valves.
The valves are crescent-shaped intimal folds consists of a connective tissue core continuous with the subendothelial connective tissue covered on both sides by endothelium. They prevent the backflow of blood in the opposite direction.
Arteriovenous anastomosis (A-V shunts)
A-V Shunts are channels that provide direct communication between arterioles and venules without passing in the capillary bed. They are similar to arterioles on their arterial side and similar to venules on their venous side.At the transition zone between arterioles and venules, the smooth muscle fibers either forms a cushion that protrudes into the lumen or is circularly arranged.
They are innervated by a dense vasomotor nerve supply. Several arteriovenous anastomosis may surround by a thick connective tissue capsules forming a structure known as glomus.Numerous nerve endings supply the glomus.
Functions
When A-V shunts open, the blood is shunted directly into the venous system bypassing the capillary bed. Therefore, A-V shunts play an important role in:
Body temperature conservation.
Regulate blood flow to the organs with intermittent activity such as intestine, erectile tissue (penis), liver and thyroid glands.
Regulate the venous return.
Lymph vessels
The principal function of the lymph vessels is to drain excess fluid called lymph from the extracellular spaces and returns it to the blood. Blind-end lymph capillaries that converge to form progressively larger lymphatic vessels drain the excess fluid (lymph). They are similar to veins. They have numerous delicate valves similar in their structures to those of the venous valves.
Lymph capillaries
They have the same structure as blood capillaries except:
Lymphatics do not contain RBCs.
They have discontinuous basal lamina.
They have a wider lumen and irregular diameter.
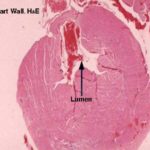
The heart is a muscular, rhythmically contracting organ pumping the blood into the vascular system.The wall of the heart consists of three main layers: endocardium, myocardiuum and epicardium.
The endocardium is the innermost layer corresponding to the tunica intima of the blood vessels.
It consists of endothelium, subendothelial layer and sunendocardial layer.
The endothelium is a single layer of flattened epithelial cells rests on a basal lamina and is continuous with the endothelium of the vessels entering or leaving the heart.
The subendothelial layer is a dense connective tissue layer contains fibroblasts, collagenous, elastic fibers and few smooth muscle cells.
The subendocardial layer is a loose connective tissue layer binds the endocardium to the myocardium. It contains blood vessels, nerves and branches of the conduction system of the heart.
![]() The myocardium is the middle muscular layer corresponding to the tunica media. It is made up of cardiac muscle cells embedded in loose connective tissue that contains a dense capillary network. Three types of cardiac muscle cells exist contractil cells, myoendocrine cells and Purkinje fibers.
The myocardium is the middle muscular layer corresponding to the tunica media. It is made up of cardiac muscle cells embedded in loose connective tissue that contains a dense capillary network. Three types of cardiac muscle cells exist contractil cells, myoendocrine cells and Purkinje fibers.
The contractile cardiac myofibers are the most numerous type. They are striated, branched and arranged in spiral bundles.
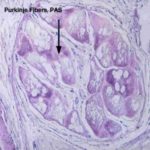
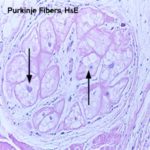
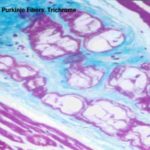
The Purkinje fibers represent the terminal branches of the impulse conducting system.
The myoendocrine cells are contractile myocardiocytes posses a well-developed secretory apparatus within their cytoplasm.
The secretory apparatus composed of scarce rER tubules, a well-developed Golgi and large number of secretory granules.
These cells are concentrated primarily within the atrial wall especially the right atrium. Recent studies have proved the presence of these cells among the ventricular cardiomyocytes. Myoendocrine cells are the primary source of a novel polypeptide hormone called atrial natriuretic peptide (ANP). ANP induce diuresis (increase excretion of water from the body), natriuresis (increase excretion of sodium from the body) and vasorelaxant effect. ANP is a potent hypotensive agent and plays a crucial role in the regulation of body fluid and electrolytes homeostasis.
The Epicardium is the outermost layer and consists of outer mesothelium and subepicardial layer of fibroelastic connective tissue supports the mesothelium.
The subendocardial layer is connected to the myocardium by a broad layer of adipose connective tissue containing branches of the coronary vessels and autonomic nerves.
The cardiac skeleton is a dense connective tissue layer to which atrial and ventricular myocardiocytes are inserted and cardiac valves are connected. It includes the annuli fibrosi or fibrous rings, the trigonum fibrosum and the interventricular septum.
The fibrous rings are dense connective tissue rings surround the atrioventricular openings and those of the aorta and the pulmonary artery. They serve to support the valves (mitral, tricuspid and semilunar valves.The trigonum fibrosum is a dense irregular connective tissue that fills the space between the atrioventricular opening and the base of the aorta. It is fibrocartilage in dog, hyaline cartilage in horse and bone in large ruminants.
The interventricular septum consists of collagen bundles between the ventricles.
Impulse conducting system
It is a network of modified cardiac muscle cells serve to initiate and coordinate contraction of the myocardium. It consists of sinoatrial node, atrioventricular node, atrioventricular bundles or bundles of His and Purkinje fibers.
The Sinoatrial node (pacemaker region) is the place at which impulses for cardiac contraction are generated. It is located at the boundary between the right atrium and the anterior vena cava.
It is composed of a network of thin, branching nodal muscle cells that contain numerous ribosomes, mitochondria and few myofibrils.
The nodal cells are embedded in large amount of highly vascular connective tissue containing many sympathetic and parasympathetic nerve fibers.
From the SA node, nerve impulses are generated spontaneously at regular intervals.
However, the rate of the nerve impulses can be modulated by the autonomic nervous system.
The parasympathetic decreases the heart rate and the sympathetic increases the heart rate. The nerve impulse spreads throughout the atria causing them to contract forcing blood into the ventricles.
The atrioventricular node is located in the lower part of the interatrial septum.It has the same structure as the SA node.
It receives stimuli from the SA node and passes them rapidly to the entire ventricular myocardium via the atrioventricular bundle.
The Bundle of His divides within the interventricular septum to give rise to smaller branches called Purkinje fibers.
The Purkinje fibers ![]()
![]()
![]() are similar to cardiac muscle cells except:
are similar to cardiac muscle cells except:
- They are larger.
- Sometimes binucleated.
- Pale cytoplasm with few peripherally situated myofibrils.
- Cytoplasm is rich in glycogen and mitochondria.
- IRIS Readiris 11 Pro
- Macrabbit CSSEdit 2 MAC
- ARTS PDF Aerialist
- AutoCAD Structural Detailing 2015
- Pinnacle Studio 17 Ultimate
- Has no T-tubules.
- Connections between the Purkinje fibers occur via
- desmosomes and gap junction rather than by intercalated discs