- Figure 1
- Figure 2
- Figure 3
- Figure 4
- Figure 5
- Figure 6
- Figure 7
- Figure 8
- Figure 9
- Figure 10
- Figure 11
- Figure 12
- Figure 13
Respiratory System
The respiratory system consists of air conducting portion and respiratory portion.
The air-conducting portion includes nasal cavities, nasopharynx, larynx, trachea, bronchi and bronchioles.
The respiratory portion comprises respiratory bronchioles, alveolar ducts, alveolar sacs and alveoli.
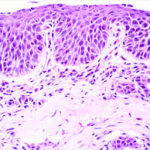
The nasal cavity is subdivided into vestibular, respiratory and olfactory regions. The vestibular region is lined by cutaneous mucous membrane. The lamina epithelialis is stratified squamous nonkeratinized that rests on a connective tissue (CT) propria-submucosa. The propria-submucosa is a dense irregular CT containing seromucoid glands; dense capillary network, immunocompetent cells, short coarse hairs called vibrissai, sebaceous and sweat glands in some animals. The respiratory region is lined by respiratory mucous membrane.
The lamina epithelialis is pseudostratified columnar ciliated with goblet cells (typical respiratory epithelium or TRE).
The propria-submucosa contains seromucoid glands, venous blood spaces as well as immunocompetent cells.
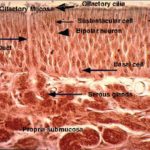
The olfactory region is lined by olfactory mucosa. ![]() The olfactory mucosa is composed of olfactory epithelium
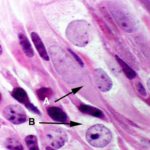
The olfactory mucosa is composed of olfactory epithelium ![]() , which is extremely tall, pseudostratified columnar in form and contains cells of three types: olfactory receptor cells, supporting (sustentacular) cells and basal cells.
, which is extremely tall, pseudostratified columnar in form and contains cells of three types: olfactory receptor cells, supporting (sustentacular) cells and basal cells.
The olfactory cells are bipolar neurons, the cell bodies of which are located in the middle stratum of the olfactory epithelium.
The apical portion of the olfactory cells extends to the free surface as a thin dendritic process where it terminates as a small swelling called olfactory bulb. The olfactory bulb gives rise to from six to eight olfactory cilia that lie flattened against the epithelial surface. The olfactory cilia are non-motile and atypical in their structure and are thought to be the site of interaction between the odiferous substances and the receptor cells. The basal portion of the olfactory cells gives rise to a single fine, non-myelinated axon which penetrate the basement membrane to join the axons of other receptor cells forming small bundles that are directed to CNS.
The supporting or sustentacular cells are elongated cells with narrow bases.
Many long microvilli extend from their luminal surfaces to project in a layer of seromucous that cover the entire epithelium. Their nuclei are oval lightly stained and located in the upper stratum of the olfactory epithelium.
Their cytoplasm contains yellow to brown pigments that give a yellowish-brown color to the olfactory mucosa. At the luminal surface, typical junctional complexes bound the plasma membranes of the sustentacular and olfactory cells. The basal cells are small, conical cells that are irregularly disposed between the bases of other cell types. They may represent epithelial stem cells.
The olfactory epithelium is supported by a vascular loose connective tissue containing bundles of afferent nerve fibers and numerous serous glands (of Bowman) which produce watery secretions in which odiferous substances are dissolved.
Functions of nasal mucosa
Air conduction.
Air conditioning (humidifies and warms inspired air).
Defense through the presence of immune cells.
Olfaction through the presence of olfactory cells.
Nasopharynx
Its structure resembles those just described for the respiratory region of the nasal cavity. The lamina epithelialis is of respiratory type (pseudostratified ciliated columnar epithelium resting on fibro-elastic lamina propria-submucosa rich in immunocompetent cells.
Along the midline of the posterior wall of the nasopharynx, there is a single pharyngeal tonsil that is made up of a group of lymphoid nodules and diffuse lymphatic tissue in intimate association with the pseudostratified columnar ciliated epithelial lining of the nasopharynx.
The laryngeal wall is made up of mucosa-submucosa, laryngeal cartilage, laryngeal muscles and adventitia. The laryngeal vestibule, epiglottis and vocal folds are lined by non-keratinized stratified squamous epithelium.
All the epithelia lining of the larynx below the vocal folds is of respiratory type.
The lamina propria-submucosa: is formed of fibroelastic connective tissue containing seromucoid glands.
The laryngeal cartilages are represented by plates of hyaline and elastic types and are bounded together by connective tissue continues with that of the propria- submucosa.
The skeletal muscles are either intrinsic muscles that join the adjacent cartilage together or extrinsic muscles that originate in the extra-laryngeal structures and insert on the cartilage of the larynx.
The adventitia is a loose connective tissue that covers the larynx from outside.
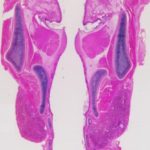
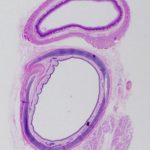
Trachea and Extra-Pulmonary Bronchus ![]()
The tracheal wall is formed of mucosa-submucosa, tracheal cartilage, loose connective tissue adventitia as well as dorsally seated tracheal muscle.
The lamina epithelialis is pseudostratified columnar ciliated with goblet cells.
The lamina propria is formed of fibroelastic connective tissue with many immunocompetent cells, blood vessels, and nerves.
The lamina propria is separated from the submucosa by a dense elastic membrane. The submucosa is a loose connective tissue layer containing simple branched tubuloacinar seromucoid tracheal glands.
The ducts of these glands empty onto the inner tracheal surface.
The tracheal cartilage is represented by a series of C-shaped rings of hyaline cartilage that help to prevent tracheal collapse during inspiration.
The transverse tracheal muscle is a smooth muscle band that extends transversely between the free ends of the cartilage rings. It is found either externally (carnivores) or internally (other animals).
The adventitia is a loose connective tissue layer covers the external tracheal surface.
The basic structure of intra-pulmonary bronchus is similar to that of the trachea and extra-pulmonary bronchus, but it differs in:
The respiratory epithelium is less tall and contains fewer goblet cells.
The lamina propria is denser and more elastic.
The lamina propria is separated from the submucosa by a discontinuous layer of smooth muscle that becomes more prominent further down the tract.
The submucosal layer contains fewer seromucous glands.
The cartilage is arranged into flattened, interconnected plates rather than C-shaped rings.
Bronchioles are airways of less than on millimeter in diameter and have no cartilagenous support.
The epithelium is formed of ciliated and non-ciliated cells with few goblet cells.
Goblet cells are completely absent beyond the terminal bronchioles.
The non-ciliated bronchiolar cells (Clara cells) are columnar with a rounded apex that may project above the other cells and carry microvilli.
Their apical cytoplasm contains secretory granules and their nuclei are central and oval. The function of Clara cells is still obscure.
Some authorities suggests a secretory role (secrete glycosaminoglycans and cholesterol) others proposed that Clara cells may act as progenitors for bronchiolar ciliated cells.
The bronchiolar wall is characterized by absence of cartilage, absence of glands and the smooth muscles do not form a continuous layer.
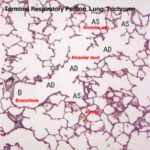
Respiratory Portion
The respiratory portion comprises respirator bronchioles, alveolar ducts, alveolar sacs and alveoli.
Respiratory bronchioles
The respiratory bronchioles resemble in its structure to terminal bronchioles except that their walls contains a small number of single alveoli.
The epithelium of the respiratory bronchioles is devoid of goblet cells and consists of cuboidal ciliated cells and smaller number of non-ciliated Clara cells.
Clara cells become the predominant cell types in the most distal part of respiratory bronchioles.
Each respiratory bronchiole divides into several alveolar ducts.
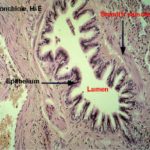
Alveolar duct and alveolar sac ![]()
![]()
The alveolar duct is a duct like structure into which many alveoli open.
In histological sections, the walls of the alveolar ducts appear as small aggregations of smooth muscle cells and associated collagen and elastic fibers.
The alveolar ducts lead to the alveolar sacs, which are sac like structure into which many alveoli open.
The alveoli are pocket like structures, open at one side and lined by extremely flattened epithelial cells, the alveolar epithelium.
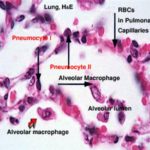
The alveolar epithelium consists of cells of two types: squamous alveolar cells or type I pneumocytes, cuboidal alveolar cells or type II pneumocytes and alveolar macrophages.
Squamous Alveolar Cells (Pneumocyte type I)
They are squamous with flattened nuclei protrude slightly into the alveolar lumen.
The cytoplasm is scanty and fads out into very thin extensions, contains few organelles.
Cuboidal Alveolar Cells (Pneumocyte type II)
They are cuboidal and fewer in number than type I cells.
The cytoplasm is vaculoated rich in organelles and osmiophilic granules.
These cells have two functions. First, they are a reserve cell, which may as needed differentiate into new squamous cells to repair damage. Second, they produce surfactant, a lipid rich material that coats the inside of the lungs and reduces the surface tension of the thin aqueous film that covers the cells.
Surfactant is necessary to keep the very small alveoli from collapsing under the surface tension of their water film, which is considerably greater than their mechanical strength.
Surfactant intercalates itself between water molecules and lessens their intermolecular attractions.
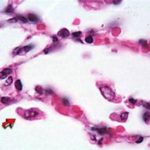
Alveolar Macrophage or Dust cells or Heart Failure cells ![]()
![]()
They are phagocytic cells originate from blood monocytes.
Its cytoplasm contains numerous inclusions such as dust particles or erythrocytes that may reach the alveolar lumen during some heart diseases (congestive heart failure).
Their role is to keep the surface of the lung as sterile as possible by taken up bacteria and any other small bits of debris which make it past the filters and dust traps in the upper regions. In disease states their numbers increase greatly as monocytes migrate to the lungs and differentiate into macrophages.
Interalveolar septum and air-blood barrier ![]()
The interalveolar septum is a thin connective tissue layer of elastic fiber reticular fibers, fibroblasts, lymphocytes, macrophoges, and many blood capillaries located between the lung alveoli.
The alveolar septa contain small opening called alveolar pores, which enable equalization of pressure between alveoli, and to provide a collateral air circulation bronchiole is obstructed.
The air-blood barrier consists of alveolar epithelium with surfactant, basal lamina of the alveolus, connective tissue fibers and cells, basal lamina of the capillary and endothelial cells of the capillary.