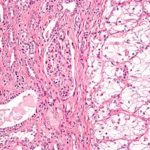
- Figure 1
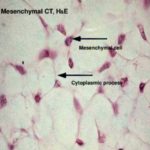
- Figure 2
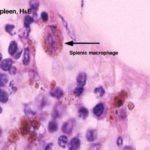
- Figure 3
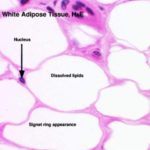
- Figure 4
- Figure 5
- Figure 6
- Figure 7
- Figure 8
- Figure 9
- Figure 10
The connective tissue proper is formed of:
1. Cells
2. Fibers
3. Amorphous ground substance
1. Connective tissue cells
The cells of the connective tissue are divided into two main groups:
Fixed or permanent cell
They have an irregular stellate shape with delicate branching cytoplasmic processes that form an interlacing network throughout the tissue. The nucleus is oval with dispersed chromatin and prominent nucleoli.
Functions
Mesenchymal cells are relatively unspecialized and are capable of differentiation into all types of connective tissue cells including that of the skeleton and smooth muscles.
Some mesenchymal cells remain in mature connective tissue and provide a source for other types of connective tissue cells.
The connective tissue macrophages may be seen in two forms: fixed macrophage or histiocytes and stimulated or active macrophage.
a. Fixed macrophages or histiocytes
It is considered one of the fixed connective tissue cells. The cells are stellate or fusiform that are difficult to distinguish from fibroblasts.
They could be differentiated from fibroblasts through:
They have smaller and darker nuclei.
They give a strong positive reaction when stained for lysosomal enzymes such as acid phosphatase.
They can be stains vitally with vital dyes such as trypan blue.
b. Stimulated or active macrophages
They are large ovoid or spherical cells with eccentric kidney-shaped nuclei and foamy cytoplasm.
At the EM level, the macrophage nucleus is indented with heterochromatin typically clumped around the nuclear envelope.
Actively phagocytic cells exhibit irregular cytoplasmic projections or pseudopodia.
The cytoplasm shows well-developed Golgi apparatus, abundant lysosomes, many phagosomes and residual bodies, a few mitochondria and variable amount of free ribosomes and rER.
Functions
Phagocytosis.
Antigen processing and antigen presentation thus participating in both humoral and cell mediated immunity.
Synthesis and secret many substances such as lysozyme (antibacterial agent), interferon (antiviral), interleukin that are essential for the proliferation of T and B-lymphocytes.
Many macrophages can fuse with each other forming large multinucleated cells called foreign body giant cells that can engulf large foreign bodies.
The macrophage and blood monocytes are considered identical. Monocytes circulate in the blood then they migrate to the connective tissue where they are called macrophages.
The macrophages are present practically in all organs, constituting a diffuse system called mononuclear phagocyte system.
They may have other names such as: osteoclasts in bone; monocytes in blood; dust cells or heart failure cells in lung alveoli; Kupffer cells in liver, and microglia in the central nervous system.
3. Pericytes 
Pericytes are elongated connective tissue cells with long cytoplasmic processes located external to the endothelium of blood capillaries and small venules.
They share a common basal lamina with the adjacent endothelial cells.
They have a fusiform nucleus and scanty cytoplasm that contains many mitochondria, rER, free ribosomes, and small Golgi complex.
Functions
The pericytes are undifferentiated cells, they serve as progenitor for fibroblasts, osteocytes, chondrocytes and smooth muscle cells.
4. Fibroblasts and fibrocytes 
Fibroblasts or fiber-forming cells are the most common type of fixed connective tissue cells. Active fibroblasts are demonstrated in healing wounds. They have large ovoid lightly stained nuclei with prominent nucleoli. The cytoplasm is
extensive and strongly basophilic with numerous interconnected cytoplasmic extensions. At the EM level, the cytoplasm is rich in rER and the Golgi apparatus is well developed.
The inactive fibroblasts (fibrocytes) are smaller and appear spindle in shape with fewer processes. At the EM level, the small quantities of cytoplasm contain sparse network of rER, poorly developed Golgi and few organelles.
Functions
Fibroblasts synthesis and secret the precursors of collagen (tropocollagen), elastin (tropoelastin), the glycosaminoglycans, and all other extracellular components.
They are the principal cells involved in wound repair and growth of connective tissue.
Free, wandering or visitant cells of connective tissue
There are two types of fat cells; white (monolocular) and brown (multilocular).
The white adipocytes are polygonal or spherical in shape. The cell occupied by a single large lipid droplet surrounded by a
thin rim of cytoplasm.
The nuclei are flattened and displaced to on side. In H&E sections, fat is dissolved during the dehydration and clearing processes.
Fat cells appear as large clear spaces surrounded by thin layer of cytoplasm giving the cells a signet ring appearance. With EM, the lipid droplet is surrounded by a thin layer of cytoplasm contains a flattened nucleus, a small Golgi
apparatus, rER and mitochondria. The lipid inclusion is not membrane-bounded, but the cytoplasm adjacent to its surface often contains microfilaments.
The white fat cells tend to occur along the coarse of blood vessels and they may also occur either singly or in-groups within the loose connective tissue layers.
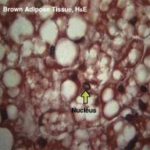
The brown adipocytes ![]() are smaller than white one, the nuclei are oval, eccentricity located and surrounded by a significant amount of strongly acidophilic cytoplasm.
are smaller than white one, the nuclei are oval, eccentricity located and surrounded by a significant amount of strongly acidophilic cytoplasm.
They could be differentiated from the white adipose tissue on the basis of:
Lipid is stored as multiple, small droplets (multilocular fat cells) that give the cytoplasm a vacuolated appearance.
Brown adipocytes have relatively large amount of cytoplasm contains abundant mitochondria that are rich in cytochromes, which give the brown color of this tissue.
Brown adipose tissue is more vascular than the white one.
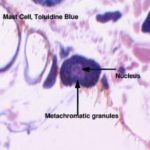
Mast cells are found in the loose connective tissues specially that of the skin and intestine, particularly in association with blood vessels. They are large polymorphic, spherical or ovoid cells with spherical centrally located
nuclei. The nuclei are completely obscured by numerous large metachromatic granules (they take a different color than that of the dye used. (e.g., when stained with toluidine blue they take red color). This property is known as metachromasia.
With EM, the granules are membrane-bounded and contain dense amorphous materials. The cytoplasm contains a prominent Golgi complex, cisternae of rER, free ribosomes and mitochondria.
Functions
The surface of the mast cell contains specific receptors for immunoglobulin E (IgE). In allergic and anaphylactic reactions, the interaction of foreign antigen with the antibody bound to the surface of mast cells induces the release of
the chemical mediators stored in mast cell granules that promote the immediate hypersensitivity reaction or anaphylaxix.
The granules of the mast cells contain histamine, heparin, ECF-A (eosinophil chemotactic factor for anaphylaxis) and serotonin in rat and mouse. The histamine causes dilatation of small vessels and increases capillary permeability. The
serotonin is a vasoconstrictor. The heparin is a potent blood anticoagulant.
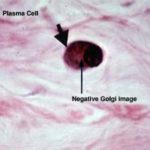
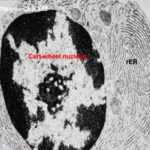
Plasma cells are spherical, oval or pear-shaped cells with spherical, eccentric nucleus. The nuclear chromatin is condensed peripherally giving the nucleus a characteristic “cartwheel” appearance. The cytoplasm is strongly basophilic
with a prominent negative Golgi image.
![]() With EM,
With EM,
the cytoplasm contains a prominent Golgi apparatus, abundant rER with dilated cisternae contain electron-dense spherical inclusion known as Russel bodies, free ribosomes and mitochondria.
They are located in the loose connective tissue specially that of the digestive, respiratory and female reproductive system. Plasma cells develop from B-lymphocytes.
Functions
Production of antibodies.
Melanocytes are derived from neural crest. They are large pigmented cells with numerous long branching processes. They occur in epidermis, uterine caruncles of sheep, meninges, choroid and iris.
5) Other connective tissue cells
They include lymphocytes, monocytes and granulocytes (especially eosinophils and neutrophils).