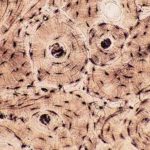
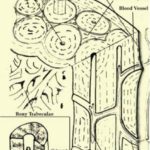
- Figure 1
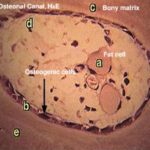
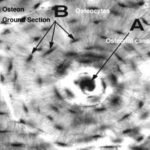
- Figure 2
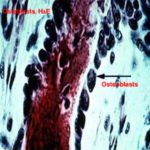
- Figure 3
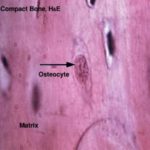
- Figure 4
- Figure 5
- Figure 6
- Figure 7
- Figure 8
Bone
The bone is a specialized form of connective tissue in which the extracellular components are mineralized. Like other connective tissues, bone is composed of cells (osteogenic cells, osteoblasts, osteocytes, osteoclasts) and matrix (a mixture of collagen fibers, ground substance and mineral salts).
- Bone cells
They are undifferentiated cells found in the endosteum, the inner osteogenic layer of the periosteum and the lining of the osteonal canal. The cells have pale-staining oval or elongated nuclei and little acidophilic or faintly basophilic cytoplasm.
They develop from the mesenchymal cells and they are capable in times of need (i.e. bone growth or fracture repair) to divide and transform into any of the other bone cells.
They are small, ovoid branching cells. During active bone formation, they are arranged in an epithelial-like layer of cuboidal cells connected to each other by short slender processes.
The nucleus is oval, eccentric (at the cells end away from the bone surface), and euchromatic with prominent nucleolus.
The cytoplasm is deeply basophilic and shows a negative Golgi image near the nucleus.
With EM, the cytoplasmic features reflect a high rate of protein synthesis with abundant rER and prominent Golgi apparatus.
Functions
Osteoblasts are responsible for the formation of organic components of bone matrix (osteoid tissue).
They secrete matrix vesicles that participate in the nucleation of crystalline bone minerals.
Resorption of osteoid tissue (unmineralized matrix).
The osteocytes are the principal cells of mature bone. They are located inside lacunae within calcified bone matrix. They are less active than osteoblasts and can not divide inside their lacunae. The cell body is flattened with numerous cytoplasmic processes that extend through tiny channels within the bone matrix called canaliculi.
The processes of the adjacent cells are interconnected with each other via gap junctions permitting flow of ions and small molecules between blood and osteocytes.
With LM, the nuclear and cytoplasmic characteristics are similar to those of osteoblasts except the Golgi region is less prominent and the cytoplasm is less basophilic.
With EM, the rER and the Golgi are still prominent, however, osteocytes situated deeper in bone matrix may have less prominent rER and Golgi saccules.
Functions
Preserve and maintain the integrity of the bone matrix.
They are large (about 50 mm) multinucleated cells lining in depressions on the bone surface called Howships lacunae. With LM, the cell has an irregular shape with an acidophilic foamy cytoplasm. The part of the cell border facing the bone surface has striated border-like structure.
With EM, the striated border seen with LM is formed of: 1) Ruffled border that is made up of branching finger-like processes projecting from the cell membrane. 2) Collagen fibrils exposed through extracellular digestion of bone matrix.
Osteoclasts originate from blood monocytes, which fuse with each other to form multinucleated osteoclast.
Functions
Degradation of mineralized bone matrix through:
Focal decalcification through production of organic acids (carbonic, lactic and citric) to generate local acidic environment capable of dissolving calcium from the bone matrix.
Extracellular digestion of the organic components of the bone matrix through liberation of acid hydrolase to the extracellular matrix.
- Bone matrix
It consists of organic and inorganic elements:
- Organic matrix
It is made up of a mixture of glycoprotein ground substance and type I collagen.
- Inorganic matrix
It consists of mineral salts, mainly calcium phosphate that is deposited as submicroscopic hydroxyapatite crystals within the collagen fibers.
Types of bone
This type forms the dense wall of the shaft or diaphysis of the long bone and is consists of the following layers:
- Periosteum
It is a tough connective tissue layer invests the outer surface of bone. It consists of two layers: a) outer fibrous layer of dense irregular connective tissue and blood vessels. b) Inner cellular or osteogenic layer formed of osteoblasts.
The periosteum is attached firmly to the bone by bundles of coarse collagen fibers that extend into the outer circumferential and interstitial lamellae of the bone and are called perforating fibers.
It is absent on the articular surface covered by hyaline cartilage and at sites where tendons and ligaments insert.
- Outer circumferential lamellae
They are bony lamellae (thin layer of calcified matrix separated by lacunae interconnected by canaliculi) arranged parallel to the outer surface of the bone.
It is the structural unit of the compact bone. It is a cylindrical structure about 0.4 mm in diameter that runs parallel to the long axis of the bone. It consists of:
- Central canal or Haversian canal
It is a longitudinal canal containing blood and lymphatic vessels and nerves.
- Haversian lamellae (or concentric lamellae)
They are about 4-20 bony lamellae that are concentricity arranged around the central canal.
- Osteocytes
They are trapped inside lacunae located within or between the concentric lamellae.
- Canaliculi
They are tiny tubules radiate from each lacuna to anastomose with those of the adjacent lacunae. The cytoplasmic processes of the osteocytes pass in the canaliculi to communicate via gap junction with the processes of adjacent cells and with the extravascular fluid in the center canal.
- Interstitial lamellae
They are bony lamellae occupying the spaces between the osteons.
- Volkman’s canal (transverse canal)
It is transverse or oblique canals connect between two Haversian canals or between the Haversian canal and periosteum. Unlike the Haversian canal, they are not surrounded by concentric bony lamellae.
- Inner circumferential lamellae
They are bony lamellae arranged parallel to the inner surface of the bone.
7) Endosteum
It invests the inner surface of the bone (marrow cavity) and is formed of only osteogenic layer that is responsible for growth of bone, continuous remodeling and fracture repair.
The cancellous bone is composed of a network of bony trabecullae separated by interconnecting spaces containing bone marrow. The trabecullae are thin and composed of bone matrix with lacunae containing osteocytes, which exchange metabolites via canaliculi with blood sinusoids in the marrow cavity.
The trabecullae are lined by endosteum that contains osteogenic cells, osteoblasts and osteoclasts. Cancellous bone forms the epiphysis of the long bone and the cores of flat and irregular bone.
Bone development
The fetal development of bone occurs in two ways:
- Intramembranous ossification
The bones of the vault of the skull and maxilla develop by intramembranous ossification that occurs within “membrane” of condensed primitive mesenchymal tissue. Mesenchymal cells differentiate into osteoblasts that begin to synthesis and secrete the organic matrix (osteoid), such areas are called centers of ossification.
The amount of osteoid is gradually increased followed by complete mineralization and some osteoblasts become trapped in lacunae to become osteocytes.
Progressive bone formation results in the fusion of adjacent bony centers to form trabecullae similar to those of cancellous bone. The primitive mesenchyme remaining between the trabecullae of developing bone differentiates into bone marrow.
As the bony trabecullae increase in width and length by addition of new lamellae, all the mesenchyme is replaced by cancellous bone that is transformed into compact bone later.
The bones of the extremities, vertebral columns develop by endochondral ossification that involves the transformation of cartilage models into bone.
Chondroblasts in the midsection of the cartilage model mature, enlarge and become separated by a very thin layer of intercellular matrix. Such region is then called a primary center of ossification.
The enlarged chondroblasts release matrix vesicles that initiate mineralization .
The deposition of calcium salts prevents the chondroblasts from receiving adequate nutrition and results in their death.
The perichondrium of the shaft assumes osteogenic potential and starts to lay down a thin layer of bone around the midsection of the cartilage model referred as periosteal band or bony collar.
After degeneration of the chondrocytes, some primitive mesenchymal cells and blood vessels invade the spaces left within the shaft and differentiate into osteoblasts.
The osteoblasts cluster around fragments of calcified cartilage and begin to secrete osteoid that is followed by mineralization. Such activity continues until bony trabecullae form that has cores of calcified cartilage. Such trabecullae are called primary spongiosa.
The capillaries from the primary center of ossification continue to invade the model toward both epiphyses that extends bone formation throughout the cartilage model.
The periosteum continues to add bone to the periphery, and the primary spongiosa in the center is resorbed by osteoclasts, thus forming the marrow cavity, which become filled with the hemopoietic tissue.
Secondary center of ossification occurs in the epiphysis of larger long bone. Ossification replaces all the epiphyseal cartilage except a transverse disk of cartilage is left between the diaphysis and epiphysis.
Growth of bone
- I) Growth in width
Bone grows in width by appositional growth. The cell in the inner osteogenic layer of the periosteum is differentiated into osteoblasts that produce new bony matrix to be added to the pre-exiting bone. Unlike cartilage, interstitial growth does not occur in bone.
- II) Growth in length
The long bone grows in length through continuous interstitial growth of the cartilage cells in the epiphyseal disk located between the epiphyses and diaphysis.
The epiphyseal disks have 4 regions:
- Zone of resting cartilage
It consists of typical hyaline cartilage with the chondrocytes arranged in small clusters surrounded by a large amount of moderately stained matrix.
- Zone of proliferation
The cartilage cells undergo successive mitotic divisions to form columns of chondrocytes separated by strongly stained glycoprotein rich matrix.
- Zone of maturation
The cell division stopped and the chondrocytes increase in size.
- Zone of hypertrophy and calcification
The chondrocytes become greatly enlarged and vacuolated and the matrix becomes calcified leading to their death.
- Zone of ossification
The osteogenic cells and capillaries from the marrow cavities of the diaphysis invade the calcified matrix. The osteogenic cells differentiate into osteoblasts that cluster on the surface of spicules of calcified cartilage matrix and start bone formation.